Do you have healthy children in your lives? If you do, do not take it for granted. Should they have the right to be healthy so they can go out in the world and be who they are meant to be? I believe they do. Society has the responsibility to provide a healthy environment for all so they can be safe, happy and productive citizens. Unfortunately, some of our young people face medical issues every day. In order for our children to be successful, we teach them the academics. We are also encouraged to empower them to take care of themselves. This is what this unit is about. Children will be looking at Asthma and how it affects them not only physically but emotionally if it is not under control. Children will learn strategies to stay healthy at home and at school. There will be a great deal of collaboration. The unit is geared for first to fourth graders. The materials utilized are easily accessible and can be differentiated for your class’ levels of abilities. The unit is for six weeks. It is a cross curricular unit designed so that every student will be successful. There will be background information for teachers on PA Act 187(2004), which states, students need to have access to their medicine. Teachers will learn local laws requiring children to have their own inhaler with them are implemented by school districts and how they districts may impose other restrictions such as keeping the inhaler with the nurse for younger children. The curriculum considers the important risks of lack of access for children in the red zone. The lessons and activities although dealing with serious content are planned to be engaging and have fun along the way.
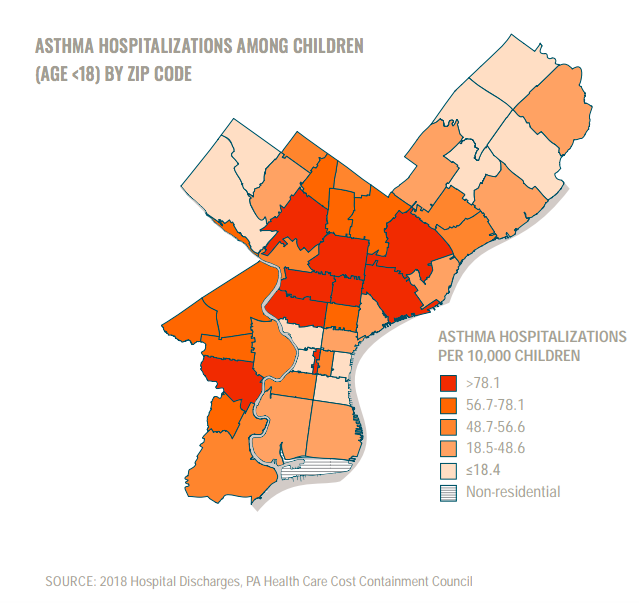
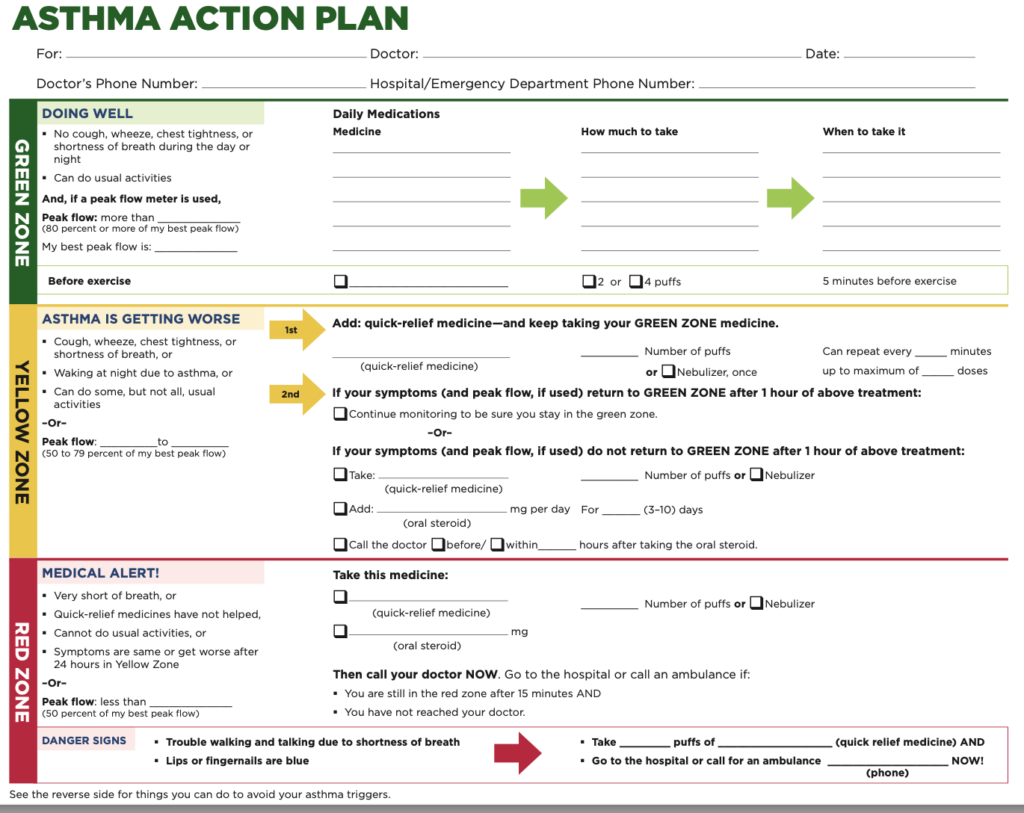
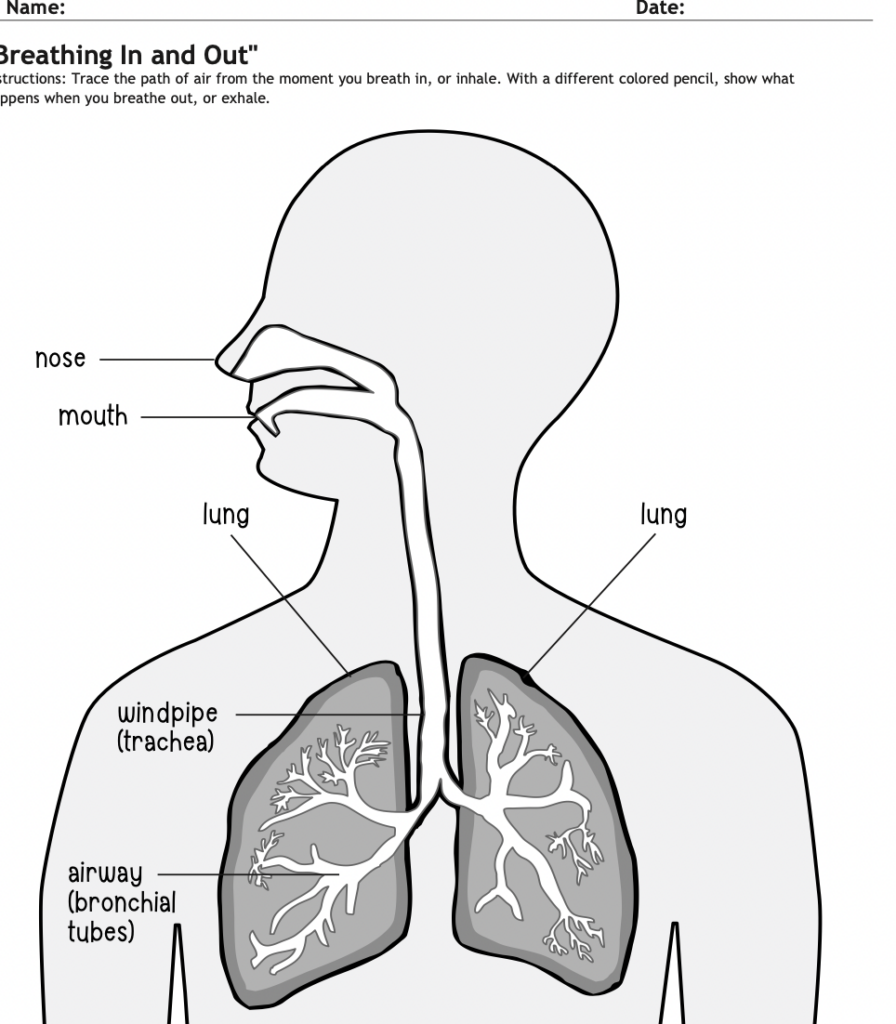
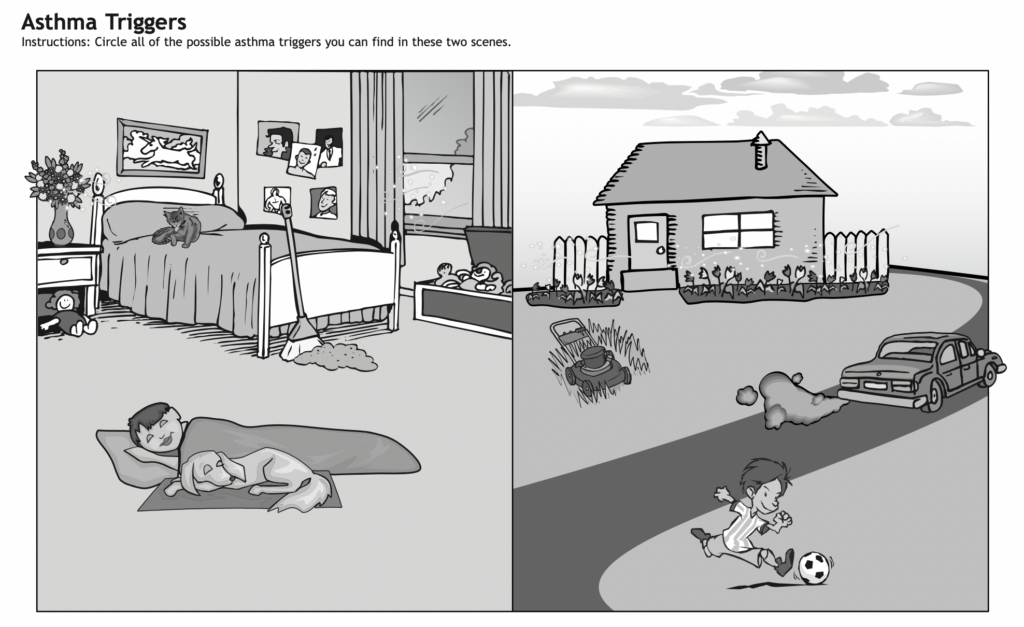
According to the World Health Organization, reducing environmental risks could prevent 1 in 4 child deaths. In 2012, 1.7 million deaths in children under five were attributable to the environment. These included 570 000 deaths from respiratory infections, 361 000 deaths from diarrhea, 270 000 deaths from neonatal conditions, 200 000 deaths from malaria and 200 000 deaths from unintentional injuries. Environmental risks have an impact on the health and development of children, from conception through childhood and adolescence and also into adulthood. The environment determines a child’s future: early life exposures impact on adult health as fetal programming and early growth may be altered by environmental risk factors. Adverse environmental conditions and pollution are a major contributor to childhood deaths, illnesses and disability, particularly in developing countries. Children are particularly vulnerable to certain environmental risks, including: air pollution, contaminated water, sanitation and hygiene, hazardous chemicals and waste, radiation, climate change, as well as emerging threats like e-waste. (World Health Organization, Climate Change and Health 2023). One of the health problems that our environment is causing is asthma. According to Dr. Tyra Bryant Stephens, a pediatric pulmonologist at Children’s Hospital of Philadelphia, 22% of children have asthma in some Philadelphia neighborhoods compared with 7% nationally (Bryant Stephens, 2012) “Overall, Black children 19 and younger are hospitalized due to asthma at a rate 5X that of white counterparts”(Philadelphia Inquirer June 8, 2023).She said, “The top priority for preventing asthma is having healthy housing and healthy schools so kids aren’t chronically exposed to allergens and irritants.”(June 8, 2023) In this unit I will be concentrating on asthma and the effects it has on children’s lives especially on their education. I will also investigate the various policies that are in place for children and also the solutions that can be implemented to help our children and families dealing with asthma. What is asthma? Asthma is a chronic lung disease that causes the airways to be inflamed, leaving less room for air to move through the lungs (CDC, asthma). In a person with asthma, the muscle of the bronchial tubes tighten and thicken and the air passages become inflamed and mucus filled making it difficult for air to move. Normally the muscles around the bronchial tubes are relaxed and the tissue thin allowing for easy breathing (See Appendix A). Here is what the bronchioles look like (Appendix B). This can cause trouble breathing and attacks of coughing, wheezing and chest tightness. Left untreated, asthma attacks are dangerous and can lead to death. What are the symptoms of asthma? The early warning signs are: Less obvious signs are: Other serious signs to look out for are: These symptoms must be carefully monitored. Emergency warnings are very fast breathing, accelerated heart rate, pale or blue face, retractions in the ribs or neck, difficult talking (cannot count to 10 in one breath), and difficult walking. It is important to listen to the child. Getting emergency care at this point can be lifesaving. Even though there is not a cure for asthma, there are medications that can be utilized to make asthma exacerbations infrequent. There is a metered dose inhaler with a facemask spacer (for babies and toddlers) and a metered dose inhaler with a mouthpiece spacer (for older children). The use of the spacer is more effective than using the inhaler alone, because more of the medicine ends up in the child’s airways where it is needed instead of the back of the throat. Another way to get medication is the nebulizer machine which creates a constant mist of medication. When your child has a severe asthma attack, they need medication fast. The quickest way to get it into their lungs and help them breathe easier is to use a nebulizer. Most families do not have a nebulizer so they take the child to the hospital when a nebulizer is needed. Here’s how it works. If an infant or child suffers from asthma and has experienced bouts of desperate coughing and gasping for air, these episodes can be scary and traumatizing. During an attack, only one thing matters — fast, effective relief. But inhalers, although portable and quick-acting, can be tricky for some kids to master so that is why they need a spacer. If the inhaler with a spacer does not seem to be working, that’s where the nebulizer comes in. Also known as a breathing treatment, nebulizers are reserved for severe asthma attacks. (The Center for Advanced Pediatrics, when would I need a Nebulizer Treatment? June 2022). How does it work? Nebulizers turn liquid medication into an aerosol so anyone who is having a severe attack and has difficulty inhaling deeply as is required to use an inhaler (even adults) can breathe in the fine mist and get rapid relief. A nebulizer isn’t portable like an inhaler; it runs on electricity and needs to be connected to an outlet. The nebulizer machine transforms the medication into a fine mist and transports that mist through a tube and into a mouthpiece or face mask, delivering breathable medication that gets into the lungs quickly and requires no training. Let us look at the various types of medications. One is corticosteroids. Children with infrequent asthma exacerbations can take this. Corticosteroids reduce inflammation in the airways and prevent asthma symptoms, such as wheezing and difficulty breathing. Corticosteroids such as beclomethasone and fluticasone come in a metered dose inhaler, a small canister that provides a measured amount of the corticosteroid. The inhaler is attached to a special delivery system, called a spacer, which collects the medication in a chamber before your child inhales it using an attached mouthpiece. Side effects, such as irritation of the throat, are usually avoided when corticosteroids are delivered with a spacer device and more of the medication is delivered to the lungs where it can be effective. Children may use inhaled corticosteroids daily to prevent asthma exacerbations. Doctors may prescribe inhaled long-acting beta agonists, such as salmeterol and formoterol, which relax muscles inside the airways for up to 18 hours. Doctors often prescribe an inhaler combining one of these medications with a corticosteroid for children whose severe asthma symptoms have not been controlled with an inhaled corticosteroid alone or for children with severe exercise-induced asthma. It’s very important to take these medications daily and not just when symptoms are present because they work to prevent symptoms. Leukotriene inhibitors, such as montelukast, block the activity of leukotrienes—one of the chief substances in the body that cause inflamed and narrowed airways in people with asthma triggered by allergies. Asthma symptoms not well controlled by an inhaled corticosteroid may respond to this medication, which is taken daily by mouth as a chewable tablet. Symptoms sometimes flare up when a child is exposed to viruses, cigarette smoke, or other triggers, even when asthma is well controlled by controller medication. Rescue medications can provide fast-acting, short-term relief of symptoms that come on suddenly. The most commonly used rescue medications are short-acting beta agonists, such as albuterol, which can be delivered to the airways in less than 30 seconds with a metered-dose inhaler. Rescue inhalers are commonly prescribed by doctors for children with asthma. Children, their parents and caregivers should know how and when to use them. Using rescue inhalers more than once a week may be a sign that a child’s asthma is not under control. Side effects of rescue medications may include jitteriness and a rapid heartbeat. Children with severe asthma symptoms may be treated briefly with a corticosteroid, such as prednisone, taken by mouth. Doctors carefully monitor children taking steroids in pill form, because they have the potential to cause serious side effects, such as slowed growth or osteoporosis, a weakening of the bones. (Hassenfield Children’s Hospital at NYC Langone). Albuterol is used to prevent and treat difficulty breathing, wheezing, shortness of breath, coughing, and chest tightness caused by lung diseases such as asthma and chronic obstructive pulmonary disease (COPD; a group of diseases that affect the lungs and airways in adults). Albuterol is in a class of medications called bronchodilators. It works by relaxing and opening air passages to the lungs to make breathing easier. Albuterol inhalation aerosol and powder for oral inhalation is also used to prevent breathing difficulties during exercise. Albuterol inhalation aerosol (Proair HFA, Proventil HFA, Ventolin HFA) is used in adults and children 4 years of age and older. Albuterol powder for oral inhalation (Proair Respiclick) is used in children 12 years of age and older. Albuterol solution for oral inhalation is used in adults and children 2 years of age and older. Albuterol inhalation may cause side effects. Parents should inform a child’s doctor if any of these symptoms are severe or do not go away: Children have different triggers. What is a trigger? Triggers are things that make asthma symptoms worse. Avoiding triggers is one step children can take to help keep their asthma under control. It is important for them to know their triggers. There are outdoor and indoor triggers. Here are some examples of outdoor triggers. They are: Weather, air pollution and pollen. Pay attention to radio, television, the internet, or newspaper reports about things that might trigger your asthma. These might include reports about weather, air quality, pollen count, or wildfire conditions. Housing conditions are responsible for many of the indoor asthma triggers that people experience. Everyone has the right to a standard of living adequate for the health and wellbeing of himself and of his family, including food, clothing, housing and medical care. (The universal declaration of human rights). This statement is so right on. If politicians focused on the needs of people, a lot of these issues that people are living with in our world would not be happening. We need to put people first. Our children’s lives are in jeopardy. The indoor triggers are: dust mites, cockroaches, rodents, indoor mold, and pets. Strategies to reduce these indoor triggers include using an air purifier with a high-efficiency particulate air (HEPA) filter and using HEPA filters for vacuum cleaners. Keeping homes clean by wet dusting and wet mopping reduces dust in the air. People who have asthma should avoid cleaning themselves but instead, ask someone else to clean their home regularly. Wearing an N-95 dust mask while cleaning may be helpful. Cleaning can actually spread asthma triggers or worsen your indoor air quality. Some tools like feather dusters only move dust around, which can spread dust mites and small particles through the air. Some vacuum cleaners can leak air, spitting the particles from your carpet right back into the air. Then there’s cleaning products. The very solutions that are used for cleaning can actually cause asthma symptoms. The Asthma and Allergy Foundation of America recommends simple soap and warm water can be effective in many cases for general cleaning. But you’ll want to use something else to disinfect (kill germs). Homemade cleaning recipes using baking soda, vinegar, borax, hydrogen peroxide, or dish soap may be less likely to cause asthma symptoms. Some people who are sensitive to scents prefer to use steam cleaners to clean (steam can also trigger asthma). Some homemade cleaning recipes call for using essential oils, like tea tree oil. But essential oils can actually be an asthma trigger because of their strong scents, and they release VOCs. (Cleaning when you have Asthma-The Dirty Truth, March 21). Many cleaning products contain strong scents, chemicals, and volatile organic compounds (VOCs) that can trigger asthma. For more information on safer cleaning products, check out the EPA safe products website (https://epa.gov/safechoice).Cleaning should not be done while children with asthma are present. Pet dander can be the asthma trigger or pets can bring other asthma triggers inside. Dust mites (tiny bugs that live in dust and fabric, especially bedding) Keep bait away and out of reach of children and pets. Avoid sprays and foggers as they are more toxic and less effective. Mold is everywhere. A small amount of mold is not a problem for health. When mold grows out of control such as after a leak or where there is a chronic leak, that is when it becomes a problem. Empty and clean refrigerator and air conditioner drip pans regularly. Another type of trigger in the home is that every day, we use soaps, lotions, deodorants, hair products and cosmetics on various parts of our bodies. But in recent years, an increasing number of reports have raised concerns about many of them. Most American children are also exposed to toxic chemicals — from a wide variety of sources — that may be a cause of learning and developmental disorders, obesity and asthma. (Knvul Sheikh, Feb 15th, 2023-The New York Times). What do you do? People can select safer personal care products at the Environmental Working Group’s website (https://www.ewg.org/skindeep/ ) . Your home should be a place of safety. Many homes in the Philadelphia area are old, and also many low-income families reside in those homes. This is a concern because homes in disrepair will cause harm to one’s health. However, in Philadelphia there is a program called Built to Last that has come to the rescue. Built to Last is a program from the Philadelphia Energy Authority. PEA began its first pilot in late 2021 to serve its first 50 homes and began its second phase of 50 homes in early 2023. PEA created the program as a one stop shop whole home repair program to serve Philadelphia homeowners. Built to Last brings together Philadelphia home repairs, energy conservation and healthy homes programs to make homes more affordable, healthier and safer. (https://philaenergy.org/programs-initiatives/built-to-last/). Another organization that is helping to keep our homes healthy is Healthy House. Their mission is to rebuild people’s health by minimizing environmental exposures. “We follow the laws of nature. When ecology thrives, biology thrives and vice versa”. (https://healthyhouse.com/mission). I mentioned the indoor triggers in the home. What about when children are at school? Students with asthma face a number of problems related to school. Teachers should know when children in their class have asthma and should collaborate with the child, parents, school nurse and coach to understand their triggers and the guidance contained on an asthma action plan. If asthma symptoms are causing any of the following problems, make sure to let the parents and school nurse know: Physical activity is important for your child’s physical and mental health. Children with asthma should be able, and encouraged, to participate completely in physical education, sports, and other activities in school. All students should have some knowledge of asthma basics and management. Encourage your school to offer asthma awareness education as part of the health education curriculum. What can the school do to make sure it is an asthma friendly school? The American Lung Association developed this quiz. (Nov 2022) Yes / No Yes / No Yes / No Yes / No Yes / No If you said “Yes” to all of the questions above, your school is on its way to being asthma-friendly. Also, the air quality is vital too. The air children breathe in school is critical to their success in the classroom and their overall health. Indoor air quality impacts student attendance, test scores and student and staff productivity. The Lung Association provides key guidance and tools for parents and school staff to identify and solve air quality issues in schools. Understanding what makes indoor air unhealthy and the specific pollutants that might be present in schools is the first step to addressing the problem. Schools face special challenges in providing healthy indoor air. School buildings are crowded places. They may have four times as many occupants per square foot as office buildings. The multiple uses of school space, including classrooms, cafeterias, gyms, art rooms and labs mean many potential sources of indoor air problems. School budgets are often tight, which may affect regular maintenance and cleaning practices. However, failure to address indoor air quality issues and take steps to prevent issues can cause problems for schools, such as: Taking steps to address air quality issues in schools before they become a problem can make a big difference in the health and success of students, faculty, and staff. Making even minor changes can have a large impact on health and learning. Increasing outdoor ventilation rates can result in higher standardized test scores, reduce the spread of respiratory illness, and decrease absences. Good indoor air quality helps to create a healthy learning environment and results in better health and learning outcomes. (American Lung Association, The importance of Air Quality in Schools) Knowledge is power and, in this case, it can save a life. Consequently, children and those who care for them need to have an Asthma Action Plan. An action plan is developed with the doctor. It is divided into three zones- Green, yellow and red. The green zone provides guidance for when the child is doing well, no coughing, wheezing chest tightness or shortness of breath. In the yellow zone, there are one or more of these symptoms: coughing, wheezing, chest tightness, breathing trouble, and waking up at night due to asthma. Or, if a child can only do some, but not all usual activities, they are in the red zone, EMERGENCY! very short of breath. Quick-relief medicines have not helped, or symptoms are the same or worse after 24 hours in the Yellow Zone. Or, if you cannot do any of your usual activities. Each section has the type of medicine that is taken and how much. (See Appendix C). In the Philadelphia School District, they may not use this particular form, but there is one that the doctors, parents and nurse have to sign off on. There is also a section where with parents input, will determine if that child is responsible enough to have the inhaler on their person. According to PA Act 187 2004, students need to have access to their medicine. Why is there so much asthma in the Philadelphia Region? According to the Centers for Disease Control and Prevention, 5.8% of children in the U.S. have asthma. This rate is more than triple for Philadelphia children, with an asthma prevalence rate of 21%. In 2020, non-Hispanic Black and Hispanic children had over 4 times more asthma related hospitalizations in Philadelphia compared to non-Hispanic White children. Asthma disparities may be explained by a combination of genetics and social determinants of health which include where children live, grow, learn and play. This map shows where in Philadelphia asthma hospitalizations, a sign of poorly controlled asthma, is prevalent. Asthma affects a child’s health as well as their academic performance. Asthma-related school absenteeism affects the majority of children with asthma and is linked to lower academic performance, especially among urban minority youth. Asthma is also a leading cause of emergency room visits for children. In Philadelphia, the rate of asthma related hospitalizations is 59 hospitalizations per 10,000 children. (A Look at Children’s Environment Health in Philadelphia, Oct 8, 2021). Let us take a look at policies that are Asthma related. In order to ensure that a child has his or her asthma medication immediately available when an asthma attack occurs, Pennsylvania has enacted a law (Act 187) requiring schools to develop a written policy that allows school aged children to carry (possess) and use (self-administer) their asthma medication. I soon learned that individual school policy may modify how the law is applied. However, each school policy should require that the child be able to demonstrate the ability to use the inhaler, behave responsibly when using the inhaler and notify the nurse immediately following the use of the inhaler. Also, a written statement from the child’s health care provider that provides the following information is required: the name of the medication, the dose, the times when medication is to be taken, the diagnosis or reason medicine is needed (unless this is confidential) information on serious reactions that could occur and appropriate emergency responses, that the child is qualified and able to self-administer the medication. There is a written statement from the parent stating that if the school follows the health care orders, school employees are relieved of any responsibility for the benefits or consequences of the prescribed medication, the school bears no responsibility for ensuring that the medication is taken (An official Pennsylvania Government Website). If the parent, health provider and nurse, believe the child is not responsible enough to have an inhaler on his person, they have to sign off on it. I have concerns with this, because what if a child has an asthma attack in class? What should I do? Will the nurse be able to get to us in time? I believe if the child has severe asthma, the inhaler should be in the classroom in a secure place of course. Another policy The School-Based Allergies and Asthma Management Program Act increases grant preference to states which implement comprehensive school-based asthma and allergy management programs (SAMPRO) that include student action plans, and education and training for school staff to administer medications in an emergency. (Allergy and Asthma Network). Another federal policy is the Clean Air Act. Here is a summary of it from the Environment Protection Agency. 42 U.S.C. §7401 et seq. (1970). The Clean Air Act (CAA) is the comprehensive federal law that regulates air emissions from stationary and mobile sources. Among other things, this law authorizes EPA to establish National Ambient Air Quality Standards (NAAQS) to protect public health and public welfare and to regulate emissions of hazardous air pollutants. Although this law is designed to protect public health it sets air standards that are changed only when the science is clear leading to many years of exposure that could have been prevented. It does not regulate indoor air. What is the cost and social impact of treating asthma? According to the World Health Organization, in 2004, the world total asthma costs probably exceeded those of tuberculosis and HIV/AIDS combined. (World Health Organization). The relation between direct and indirect asthma costs is variable and depends on country and type of study. Most asthma studies performed in the last 2 decades showed that direct costs are higher than indirect costs. Usually, directs costs contribute to 50 to 80% of the total costs. Direct cost include asthma management (e.g. visits to emergency services; hospital admissions; medications, including all types of medications, such as over-the-counter and alternative medicines; outpatient visits, including all human resources involved, such as doctors, nurses, paramedics, psychologists…), complementary investigations or treatments (e.g. imaging, skin and blood tests, lung function tests, pulmonary rehabilitation…) and other costs (e.g. domestic or professional preventive measures, assistance in home care, transportation to medical visits…). Indirect costs include work-related losses (e.g. temporary disability in terms of partial or total lost-days; early disability; permanent disability…) and early mortality. Finally, intangible costs are those related with unquantifiable losses, such as the decrease in quality of life, increases in pain or suffering, limitation of physical activities and job changes. These costs, unfortunately, are not yet systematically included in the literature on asthma costs. A lot of studies reported data on asthma costs, either at the individual patient, or on the society (regional or country level), and it can be an average annual per-asthmatic cost of about $USD 5,000, being much higher in severe asthmatics. (Nurmagambetov et al., 2018). Individuals with asthma can have restricted working days or, in many cases, need for time off for rehabilitation of an asthma exacerbation; nevertheless, some of these patients need retirement or removal from their work due to incapacity to have normal productivity. How does this affect children? Multiple social determinants of health contribute to asthma disparities: low household income; environmental inequities (e.g., outdoor air pollution and substandard housing) and living in poor communities; exposure to pests, mold, air pollution (including secondhand smoke); and high levels of stress (Burbank and Peden, 2018). What about the emotional impact? In addition to the common occurrence of depression and loneliness in asthmatic children, a child with asthma is likely to experience lower self-esteem (Plaza-Gonzalez, et al., 2022). One reason is that they may never participate in sports so will not have the opportunity to set goals in this respect. As you can see, asthma needs to be taken seriously. It is in everyone’s interest to do what they can to get this issue under control. The State and Federal Government has a moral and social responsibility to improve regulation to protect everyone.
Controller Medications
Rescue Medications
What Causes Children to Have an Asthma Exacerbation?
Dust Mites:
Cockroaches, Mice, Rats
Mold /Humidity
Smoke, Sprays, Scents, Disinfectants
Coping with Asthma at School
Is your school up to the asthma-friendly challenge?
This unit will be introduced by asking students to do sixty jumping jacks. Why? I want them to say stop or even say I am out of breath. This will be my way to start the conversation by saying, imagine those children who have asthma. How do you think they feel that some days they cannot breathe as easily as us? The next question will be. Do you know any individuals who have asthma? We will do a KWHL-where K = Know, W – What you want to know, H – How to find out, and L- Learned. This will be a pre-assessment and will be kept up in the class for a resource. This unit will also lead to Social Emotional Learning. We want our children to show empathy for others. There will be many discussions and collaborations. It is imperative that students understand how to work in groups and how to listen and be heard. The teacher will model and practice with students. Talking prompts to utilize will include “Rephrasing – This is what I hear you are saying.” And “I respectfully disagree, but this is how I see it.” Students will affirm someone else’s hard work by saying “That’s a great idea.” or saying, “Marie, that was a good job.” If students need clarification, they will say, “Could you explain that again please?” Students need to face each other, maintain eye contact (if that is accepted in that culture) and stay quiet while the other person is speaking. Talking chips, talking sticks, talking bears) can be utilized to show that once your chips are finished, it is time to give another person to speak. They will have to understand that if someone disagrees with them, it is not that they do not like them, but rather that we are all entitled to our various points of view. This will mean that a safe community needs to be created for students to take chances and participate. These skills will be practiced during Morning Meetings, circle time, whatever name is being used at your school to create a class community. Other strategies that will be utilized will be turn and talk where students learn to listen and wait for their turn to speak. There is another technique called Active Learning. The steps are Reciprocal Questioning- students come up with the questions. Next is The Pause Procedure- students take a break every 10-15 minutes so they will have the time to discuss questions and solve them. Last is the Muddiest Point – students write which part of the lesson was not clear. This information will help the teacher to plan for the next lesson. In the classroom, there are various types of learners and also those with disabilities and English language Learners. As a result, the Universal Design of Learning will be implemented. This just means that lessons will be differentiated if needed. We want all students to be engaged and involved in the learning. Students will not only be listening, they will be speaking as they will be interviewing someone who has asthma. During the unit, students will read independently, share reading and also listen to read aloud of different genres. Before reading a story, students will engage in a quick Write Up, which is writing a prediction of the story. Other strategies that will be implemented before reading will be Quick Draw, Four Corners, Listening with a focus. To help to learn vocabulary words, we will play vocabulary charades or explicit teaching using the word in a sentence. Also, other strategies to teach vocabulary will be utilized, including Illustrating the words, play “Quick Draw ”, and using the words in the real world. During reading, the teacher will stop and ask various questions according to Bloom’s Taxonomy. At the end of the story, there will be Exit slips or Think Write Pair and Share. During each section of study, there will be a formative assessment to check for understanding. At the end of the unit, there will be a summative assessment. Students will be playing games which is a strategy called Learning through playing. They will also watch videos and listen to music. They will create their own music. They will also make posters and pamphlets to share the information to others. This will be a cross-curriculum. Another strategy that will be utilize is call Image Analysis: Image analysis connects students to the lesson themes and activates prior knowledge. Here, students are encouraged to use all the language they have to make connections and establish foundational vocabulary associated with core lesson themes. Image Analysis tasks should somehow signal concepts, themes, and language students will require later while simultaneously giving the teacher a sense of what students already know and associate with essential class concepts and language. How is it done? Students build vocabulary in the language of instruction by noting their observations with the language they have. Later, they can translate the terms they don’t yet know with partners or with their teacher. KWL charts are excellent tools to follow Image Analysis tasks as a way of capturing what we know as a class and what we have yet to find out.
Lesson 1 Title: Introduction to Asthma Unit Grades: 1-4 Duration: 45 minutes Standard Utilized: Social Emotional Learning Objectives: Students will have a discussion using accountable talk about asthma before going into the full study of the content. Materials: Chart Paper, markers and interview paper Procedures: Teacher will say to the class, okay everyone, it is time for a brain break. We will do sixty jumping jacks. Ready get set go. Teacher and students will do the jumping jacks. After the exercise, the teacher will ask, how are you feeling? Teacher will write students’ responses. This chart will be kept during the unit. Teacher will say, Imagine, someone who has asthma their whole lives and what they go through when they are having an asthma attack. You only did this for five minutes. Turn and Talk with a partner and talk about it. Remember, what you do when we are working with a partner- take turns speaking, listen to each other, give eye contact and if there are any disagreements, say I respectfully disagree. Also, if you do not understand, ask for clarification. Students will be given ten minutes to discuss. After the discussion, they will come together and talk with the group. During this lesson, the teacher will be more like a facilitator. At the end, the teacher will ask the class, does anyone not know someone with asthma? asthma is pretty common. Lesson Closure: In the next four weeks, we will be discussing what asthma is, the affects, the causes and solutions. I also want you to be emphatic of those with this medical condition. As a follow up to our conversation, you will interview someone who has asthma. Bring it back and we will discuss your findings. (See Appendix) Lesson 2 Title: Breathing in and Out. Grade: 1-4 Duration: 45 minutes Standards Utilize:MS-LS1-3 Structures and Processes (NGSS) Objectives: Students will identify the parts of the respiratory system in order to comprehend how asthma works. Materials: Interview Paper, Breathing in and Out (Appendix D), colored pencils video Buster Baxter- Lung Defense https://youtu.be/rP_sVpiRNsA?si=5kXrqchn8ttKgazs Procedures: Students will share what they found out from their interviews from the previous day. Teacher will write down their responses. Teacher will then today, we are going to look at how we breathe and the parts that help us to breathe. How do you think we breathe? Teacher will hand out the “Breathing in and Out” paper, where students will trace the path that air takes from the moment you take a breath, or inhale. With a different colored pencil or crayon, show what happens when you exhale, or let a breath out. Teacher will give students to explore the Buster the Lung Defender game. Lesson Closure: Teacher will ask students to explain how one breathes. Teacher will say in our next lesson we will look at asthma. Lesson 3 Title: I have Asthma Grades: 1-4 Duration: 45 minutes Standard Utilized: CC.1.2.2.B Ask and answer questions such as who, what, where, when, why, and how to demonstrate understanding of key details in a text. Objectives: Students will be able to demonstrate an understanding of a text, in order to ask and answer questions. Students will have a clear understanding of how asthma affects an individual in order to show empathy. Help children with asthma or similar conditions feel safe and accepted. (Emotional Social Learning). Materials: I have Asthma by Jennifer Moore – Mallinos Procedures: Before reading the text, the teacher will say we will meet a little boy who has asthma. I want you to put yourself in his place and think about what he is feeling. The teacher would ask for a definition of asthma. Teacher will write it on a chart. The teacher will stop at various points to check for understanding. At the end of the text, the teacher will ask questions to continue to check for understanding. Here are few samples: Lesson Closure: Teacher will review today’s lesson by saying, people who have asthma sometimes have trouble breathing. Asthma affects a person’s airways, or bronchial tubes. During an asthma flare-up, a person’s airways get narrower, making it harder for air to get to and from the lungs. It’s like having to breathe through a straw. During an asthma flare-up, a person may cough or wheeze. Lesson 4 Title: What causes Asthma and how it is treated? Grades: 1-4 Duration: 45 minutes Standard Utilized: CC.1.2.2.B Ask and answer questions such as who, what, where, when, why, and how to demonstrate understanding of key details in a text. Objectives: Students will be able to identify triggers of asthma and flare-ups in order to assist anyone in need and also how to prevent flare ups. Materials: Asthma Trigger paper, video Asthma Rap Procedures: Teacher will create a T chart. One side will have the causes and another will be Treatments. The teacher will ask students what they think it means to trigger asthma? Students will listen to their responses. the teacher will then define an asthma trigger. An asthma trigger is something that can lead to an asthma flare-up. Asthma triggers include pollen (powder made by plants to help them make more plants), smoke (from cars and cigarettes), and even animal dander (skin flakes from animals, including cats and dogs). People react to these triggers differently. What might lead to a flare-up for one person might be ok for another person with asthma. Teacher will say now that we know what the causes are, what can we do to treat it? Teacher will show pictures of inhalers and inhaler spacers. The teacher will also discuss types of medicine that can be utilized. Students will look at the pictures on the “Asthma Triggers” handout. (Appendix E) Students will circle everything you find that could trigger an asthma flare- up. After the lesson, students will listen to a video called “Asthma Rap.” https://youtu.be/VA-B4KUkEKQ?si=MFm8Gd7Wm-wlLQZg Closure: students will share in groups what they have learned. For a homework assignment student will find the triggers in their homes. The assignment is call, Going on a Trigger Hunt Lesson 5 Title: Famous people with Asthma Grades: 1-4 Duration: 45 minutes Standard Utilized:CCSS.ELA W.3.7 Conduct short research projects that build knowledge about a topic. Objectives: Students will investigate and make a report of famous people who are living with Asthma. Materials: Books and articles internet Procedures: We have defined what asthma is its causes. The teacher will point out to students that asthma doesn’t have to stop you from doing fun things. Teacher will show pictures of famous people who have asthma. They are Dennis Rodman- basketball player for the Chicago Bulls, David Beckham- soccer player and Jackie Joyner-Kersee, an athlete. We will investigate these famous people and others who live successfully with asthma. Closure: Students will be given a week to find a person who has asthma and do research on the person. Students will present their findings in a creative way. Lesson 6 Title: The Triggers (Math) Grades: 1-4 Duration: 45 minutes Standard Utilized: 3.MD.B.3 Draw a scaled picture graph and a scaled bar graph to represent a data set with several categories. Solve one- and two-step “how many more” and “how many less” problems using information presented in scaled bar graphs. For example, draw a bar graph in which each square in the bar graph might represent 5 pets. Objectives: Students will investigate the pollen level for a month in order to create a bar graph. Materials: Chrome books, newspaper graph paper, website Procedures: students will investigate the pollen level in various places using the pollen map site. (https://www.pollen.com/map). For some people, pollen in the air can trigger asthma flare-ups. With the help of the teacher, students will use the Internet or your local newspaper to keep track of pollen levels each week for 1 month. Are they (a) very high, (b) high, (c) medium, or (d) low? Make a bar graph to show the data you collected each week. Leeson Closure: Students will share and discuss their findings. Lesson 7 Title: Data Anyone? Grades: 1-4 Duration: 45 minutes Standard Utilized: 3.MD.B.3 Draw a scaled picture graph and a scaled bar graph to represent a data set with several categories. Solve one- and two-step “how many more” and “how many less” problems using information presented in scaled bar graphs. For example, draw a bar graph in which each square in the bar graph might represent 5 pets. Objectives: Students will be able to gather data in order to create a bar graph and analyze the findings. Students will investigate more of the triggers in order to identify them in the schools and homes. Materials: graph paper Procedures: Before going off, discuss what types of triggers they could find. (photocopy and scanner). Teacher will place students into groups. They will go to different locations in the school to find triggers. After gathering their data, they will make a picture or a bar graph and share their findings with the class. Combine the trigger at home with this graph. Lesson 8 Title: Air Pollution and Cost of Gas Grade: 2-4 Duration: 45 minutes Standard Utilized: Objectives: CC.1.2.3.A Determine the main idea of a text; recount the key details and explain how they support the main idea. CC.1.2.4.F Determine the meaning of words and phrases as they are used in grade level text, including figurative language. CC.3.OA.D.8 / 2.OA.A.1.solve two-step word problems using the four operations. Represent these problems using equations with a letter standing for the unknown quantity. Students will appreciate air pollution reduction by calculating the cost of gas for a week when vehicles idle. Materials: Air Pollution. Gasping for Air, Asthma and Allergies and Their Environment. (Readworks) Procedures: Students will choose one of the informational texts to add to their understanding of how asthma affects the body and also how our environment plays apart. They will answer the questions that follow. Students will calculate the cost of the gas. Closure: Teacher will follow up with the reading checking for understanding. Students will present their findings of the cost of gas over 3 days. Lesson 9 Title: Call to Action/Create a song and a poster Grades: 1-4 Duration: 45 minutes Standard Utilized:VA:Cr1.2.4a Collaboratively set goals and create artwork that is meaningful and has purpose to the makers. VA:Cr1.2.3a Apply knowledge of available resources, tools, and technologies to investigate personal ideas through the art-making process. MU:Cr3.2.3a Present the final version of personal created music to others, and describe connection to expressive intent. MU:Cr3.2.4a Present the final version of personal created music to others, and explain connection to expressive intent. Objectives: Students will be able to create artwork and music in order to convince an audience to make a social change. Materials: paint, paper poster boards Procedures: Teacher will show examples of artwork that display various call to action themes. Teacher will ask, how does this make you feel? What can we do to convince individuals to change their behavior? We are going to create pictures and post them around the school that will educate others about the effects of asthma. First you will do a draft of what ideas you will want to present. Then when it is approved, we will do the final product. This is an opportunity to collaborate with the Art and Music Teacher. Lesson Closure: Students will share work. Lesson 10 Title: Writing About Asthma. If someone you know has Asthma what are the solutions you can give them? Grades: 1-4 Duration: 45 minutes Standards utilized:CC.1.4.3.H. Introduce the topic and state an opinion on the topic. Introduce the topic and state an opinion on the topic. Objectives: Students will be able to support a point of view with reasons and information, in order to write an opinion piece. Materials: Journal paper pencils crayons Procedures: Students will use a graphic organizer to help them put their ideas together. They will then write their opinion pieces. Teacher will review parts of an opinion writing which states your opinion, give three to four reasons and an ending. Teacher will show the opinion chart starter to help those who are having a difficult starting Lesson Closure: Students will share their writing with their peers. Lesson 11 Title: Writing to State Representative And/ To the School District of Philadelphia Grades: 1-4 Duration: 45 minutes Standards utilized: CC.1.4.3.H. Introduce the topic and state an opinion on the topic. Introduce the topic and state an opinion on the topic. Objectives: Students will be able to support a point of view with reasons and information, in order to write an opinion piece. Materials: Journal paper pencils crayons Procedures: Students will use a graphic organizer to help them put their ideas together. They will then write down the triggers they have found in their schools. The teacher will state what they think will be vital information to include in their writing to convince the district to take action. Lesson Closure: Students will share their writing with their peers. Lesson 12 End of Unit Assessment: Students will create a presentation, using PowerPoint, Google slides or posters showing their understanding. They will also do an oral presentation. (Appendix G). (refer to lesson 10). Other Activities Matching Definitions Respiration, Asthma, Action Plan, Airways Environment, Medicine Narrow ___________________in the chest allows a person to breathe. ___________________helps a person keep track of their asthma. ___________________conditions around us – the air, water, soil, and living things where we live, work, go to school, or play ___________ the act of breathing – taking air into the lungs and letting air out of the lungs. ___________________happens to the airways when a person has an asthma attack. ___________________makes a person feel better and helps them get well when they are sick. Straw test Games (Sorting Game Appendix I) Lungtropolis Interview the Nurse and Building Engineer Student Activity 1: Maria’s Story – What is Asthma? Vocabulary: breathing, wheezing, asthma, symptoms, airways, narrow, asthma attack, exhale, lungs, inhale, chronic, recurring Maria got a telephone call from the nurse at her son’s school. Thomas was having trouble breathing and a wheezing sound was coming from his chest. The nurse asked if he has asthma. She noted that asthma can cause symptoms of coughing, wheezing, and shortness of breath. Asthma causes the airways in the chest to swell and get narrow or small making it difficult to breathe. She thought Thomas was having an asthma attack because he was having difficulty exhaling air from his lungs and he coughed when he inhaled air into his lungs. Maria told the nurse that both she and her son have asthma, a chronic illness that is recurring and happens again and again over a long period of time. She told the nurse that she gets scared because Thomas has asthma attacks often. He gets them at home and at school. He likes to run around outside with his friends, but his parents want him to stay inside because of his asthma attacks. It makes him unhappy. What leads to asthma attacks? Vocabulary: environment, respiration, asthma triggers, Asthma Action Plan, medicine Maria called the doctor. The doctor thought Thomas was having an asthma attack because of conditions in the environment where he lives, goes to school, or plays that affect his respiration, or ability to breathe. He gave Thomas medicine to help him breathe and asked his parents to find out what things in Thomas’s environment are causing him to have an asthma attack. The things in the environment that cause asthma attacks are called asthma triggers. The doctor helped Maria learn about asthma triggers and they filled out an Asthma Action Plan to keep track of Thomas’s asthma triggers, the medicines he needs, and what to do when he has an asthma attack. Vocabulary Practice – Defining Words Directions: Write the definitions (meanings) in your own words, from memory, by looking at the reading about asthma in Maria’s Story, or by using a dictionary. asthma: wheezing: asthma attack: chronic: asthma triggers: symptoms:
Students will practice the vocabulary words and also will make their own word find puzzle using these words related to breathing and asthma: lungs, nose, mouth, bronchioles, trachea, inhale, and exhale. Challenge a friend to solve your puzzle.
Directions: Use the following words to complete the definitions below.
Allergy and Asthma Network.https://allergyasthmanetwork.org/what-is-asthma/ Asthma Journal for Kids.(2021). Zmeg Publishing. Asthma and Allergy Foundation of America.https://community.aafa.org/blog/cleaning-when-you-have-asthma-the-dirty-truth American Lung Association. The importance of Air Quality in Schools.(2023). Bryant-Stephens T, et al. (2012) Asthma Prevalence in Philadelphia: Description of Two Community-Based Methodologies to Assess Asthma Prevalence in an Inner-City Population. J. of Asthma. 49(6): 581-585. Built to Last.(https://philaenergy.org/programs-initiatives/built-to-last/) Burbank AJ, Peden DB. Assessing the impact of air pollution on childhood asthma morbidity: how, when, and what to do. Curr Opin Allergy Clin Immunol. 2018 Apr;18(2):124-131. doi: 10.1097/ACI.0000000000000422. PMID: 29493555; PMCID: PMC6016370. Center of Excellence in Environmental Toxicology.A Look At Children’s Environment Health In Philadelphia. (2020.Oct 8). CDC, Asthma, accessed November 12, 2023.https://www.cdc.gov/asthma/default.htm Environment Protection Agency.https://www.epa.gov/asthma Hassenfield Children’s Hospital at NYC, Langone. Healthy House.(https://healthyhouse.com/mission). Nurmagambetov T, Kuwahara R, Garbe P. The Economic Burden of Asthma in the United States, 2008-2013. Ann Am Thorac Soc. 2018 Mar;15(3):348-356. doi: 10.1513/AnnalsATS.201703-259OC. PMID: 29323930.PA. Health Care Cost Containment Council.2018. Hospital Discharges Pennsylvania Government Website( Act 187).https://www.pa.gov/ Philadelphia Regional Center for Children’s Environmental Health. (2023, June) Plaza-González S, Zabala-Baños MDC, Astasio-Picado Á, Jurado-Palomo J. Psychological and Sociocultural Determinants in Childhood Asthma Disease: Impact on Quality of Life. Int J Environ Res Public Health. 2022 Feb 24;19(5):2652. doi: 10.3390/ijerph19052652. PMID: 35270342; PMCID: PMC8909745. Sheikh,Knvul(Feb 15th, 2023).Many Personal care products Contain Harmful Chemicals. Here’s what to do About it. The New York Times. The Center for Advanced Pediatrics.(2022, June). When would I need a Nebulizer Treatment? World Health Organization.(2023). Climate Change and Health . Asthma Rap- Sesame Workshop.Asthma Rap Buster Baxter:LungDefender- Arthur Games-PBS Kids.Buster Baxter: Lung Defender – Arthur Games – PBS Kids Dunbar, T.Rhyan. ( 2021). I have Asthma but Asthma Doesn’t Have Me. Royal-T Publishing Mallinos-Moore, Jennifer.( 2007). I have Asthma. Barron’s Educational Series Inc, U.S. Mitchell, Barbara & Gosselin, Kim. (1998 ).Taking Asthma to School. Jaylo Books Publisher. Pollen Map. https://www.pollen.com/map ReadWorks. (2007). Air Pollution. Weekly Reader Corporation. Thomas, Abraham. Roo with Asthma. ( 2021).How to handle an Asthma Attack. Independently published. What is Asthma? The Dr. Bincos Show.(2019). .https://youtu.be/s1R0dL1VB0I?si=SQskX1VrKXF4xZRxChildren’s Resources
Worksheet Questions: Report Back to Class: What is it like to have asthma? Sorting Game Asthma StyleAppendix A
Appendix B
Appendix C
Appendix D
Appendix E
Directions: Ask the students to share with the other students what they learned about what it is like to have asthma.Appendix F
Appendix G